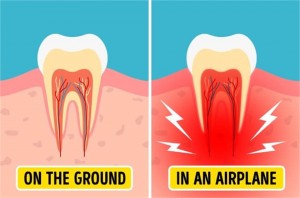
Pain in the teeth that results from a change in air pressure (as in flying or mountain climbing) . Aerodontalgia affects some person who experience pain in the tooth during high altitude flight or during deep sea diving. At ground level the tooth is completely asymptomatic. In some cases the pain may not start readily during flight or during diving, instead it may occur few hours or days later .The condition may be related to subclinical pulpitis. Sometimes similar problem may happen in an endodontically treated tooth with improper obturation of the canal. The entrapped air in an improperly obturated canal may expand during flight or driving due to alteration in atmospheric pressure. This applies pressure in periapical nerve bundle and produce pain.
Tetracycline stained teeth
Tetracycline teeth stains develop on permanent teeth while they are still forming under the gum line. During development, the drug becomes calcified in the tooth, generating tetracycline tooth stains. Children are susceptible to tetracycline tooth stains from the time they are in utero until the age of 8. Since teeth start to develop before we’re even born, pregnant women should not take tetracycline to prevent the possibility of the drug affecting the unborn baby’s oral health.Gray or brown in color, these deep, dark stains either cover the entire tooth or appear as a pattern of horizontal stripes. Because they form during tooth development, tetracycline teeth stains are embedded in the tooth’s enamel and inner layers. This classifies them as intrinsic stains — discoloration that comes from inside the tooth. Although harmless, tetracycline stains are obvious and permanent, often causing embarrassment and low self-esteem in those who suffer from them.
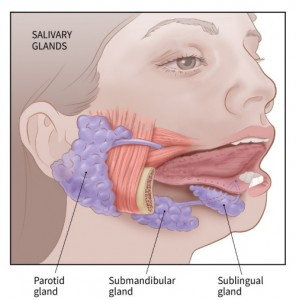
Sialadenitis
Sialadenitis is the infection of the salivary glands caused by a bacteria or virus. The parotid, located in front of the ear and submandibular, placed below the chin are the glands, which are affected most commonly. They cause ache, tenderness, redness, and steady concentrated inflammation of the region affected. It can be either acute or chronic, and is frequent among adults with salivary gland stones. However, it can occur to anyone, including infants. If not treated well, Sialadenitis can progress into a severe infection. Causes of Sialadenitis. Bacteria cause most of the acute cases, specisalivary-gland-stones1ally staphylococcus infections. Ignorance of oral hygiene is a major reason for this infection. Apart from these, infections like HIV, herpes, and mumps can also lead to the swelling of the salivary gland. Chronic Sialadenitis is often caused by salivary stones, which are nothing but deposits of calcium and different minerals that get accumulated in the glands and lead to blockages. Although less frequent, a person can also develop this infection due to the result of the immune system responding to other drugs given to treat different glandular cases.
Composite or tooth colored filings
Composite resins, or tooth-colored fillings, provide good durability and resistance to fracture in small- to mid-size fillings that need to withstand moderate pressure from the constant stress of chewing. They can be used on either front or back teeth. They are a good choice for people who prefer that their fillings look more natural.
Composites cost more than amalgam and occasionally are not covered by some insurance plans. Also, no dental filling lasts forever.
It generally takes longer to place a composite filling than it does for a metal filling. That’s because composite fillings require the tooth be kept clean and dry while the cavity is being filled. Tooth-colored fillings are now used more often than amalgam or gold fillings, probably due to cosmetics. In a society focused on a white, bright smile, people tend to want fillings that blend with the natural color of their teeth.
Ultimately, the best dental filling is no dental filling. Prevention is the best medicine. You can dramatically decrease your risk of cavities and other dental diseases simply by:
- brushing your teeth twice a day with fluoride toothpaste
- flossing daily
- eating a balanced diet
- visiting the dentist regularly.
Tooth-colored composite fillings
Advantages:
- Aesthetics — the shade/color of the composites can be closely matched to the color of existing teeth; is particularly well suited for use in front teeth or visible parts of teeth
- Bonding to tooth structure — composite fillings actually chemically bond to tooth structure, providing further support to the tooth
- Versatility in uses — in addition to use as a filling material for decay, composite fillings can also be used to repair chipped, broken or worn teeth
- Tooth-sparing preparation — sometimes less tooth structure needs to be removed compared with amalgams when removing decay and preparing for the filling
Tongue Scrapers and Cleaners

A tongue scraper is a tool used to help clean your tongue. Tongue scrapers come in a variety
of shapes and sizes, and work by starting at the back of the tongue and pulling the scraper
forward. Some people choose to clean their tongue by using their toothbrush as well.
Some say that cleaning your tongue helps keep your breath fresh, but there is no evidence that
brushing or scraping your tongue will prevent bad breath or improve halitosis (chronic bad
breath). In fact, bad breath bacteria can grow back just as fast as you remove it.
If you like the way your mouth feels after you clean your tongue, keep it up as part of your daily
dental routine. It can be a great way to go the extra mile for your mouth, but comes down to personal preference and is not a necessary step.
However, there are four things you can do to make sure your mouth is healthy:
1. Brush your teeth twice a day with a fluoride toothpaste.
2. Clean between your teeth daily.
3. Eat a healthy diet that limits sugary beverages and snacks.
4. See your dentist regularly for prevention and treatment of dental disease.
How to perform a tongue scraping to perform tongue scraping, you’ll need the right tool — a tongue scraper. A quick search for
tongue scrapers can reveal lots of options. These include ones made from plastic, copper, and
stainless steel.
Most will have a slightly rounded shape, much like an inverted spoon. If you’re in a pinch,
household items like a spoon (clean, of course) or your toothbrush will do. However, they may
not remove as much odor-causing bacteria as a dedicated tongue scraper.
To perform tongue scraping, follow these steps:
1. Stand in front of a mirror, open your mouth, and stick out your tongue.
2. Gently set the rounded end of the tongue scraper at the back of your tongue.
3. If you’re worried about gagging, you may find it helpful to start at the middle of your tongue.
You can gradually start from farther back as you get used to scraping.
4. Gently touch the scraper to your tongue. Slowly pull it forward, toward the tip of your tongue.
You should never push the scraper from the tip of your tongue back. Always go from the back of
the tongue to the tip.
5. After each scrape, use a washcloth or tissue to remove debris from the scraper.
6. Repeat until you’ve scraped the entire surface of your tongue. One to two scrapes across the
same area is usually enough.
7. Wash the tongue scraper with warm water and soap, dry, and store in a clean, dry area.
The entire process usually takes less than two minutes. Repeat as needed throughout the day.
Are there any side effects or risks to consider?
One of the biggest concerns about tongue scraping is stimulating the gag reflex. This could
make you vomit while tongue scraping.
To avoid this, refrain from placing the scraper too far back on your tongue. When you first start
scraping, you may find it helpful to scrape from the middle of your tongue to the tip. You can
gradually start from farther back as you get used to the sensation.
It’s also possible to accidentally cut the surface of your tongue with the scraper.
To prevent this from occurring, make sure your tongue scraper doesn’t have any uneven or rough
edges. You should inspect your scraper before every use to ensure that it’s still safe to use.
You should be mindful of how much pressure you’re applying. You want to be gentle enough to
avoid harming your taste buds or breaking the skin, but firm enough to scrape up excess debris.
When in doubt, start soft and gradually increase the pressure.
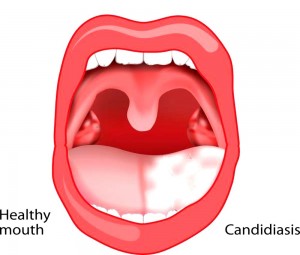
Thrush
Thrush (also called Candidiasis or moniliasis) is a fungal infection that occurs when the yeast Candida albicans reproduce in large numbers. It is common among denture wearers. Most often it occurs in people with weak immune systems—the very young, elderly or those debilitated
by disease, such as diabetes or leukemia. In addition, people with dry mouth syndrome are susceptible to candidiasis. Candida may also flourish after antibiotic treatment, which can decrease normal bacteria in the mouth.
Controlling candidiasis means focusing on preventing or controlling the condition that causes the outbreak.
Good oral hygiene is essential. Clean your dentures to remove Candida and remove them at bedtime. If the cause is dry mouth saliva substitutes and prescription medications may be helpful when the underlying cause of dry mouth is incurable or unavoidable.
What Are the Symptoms?
White, slightly raised areas in your mouth are common signs of thrush. They’re usually found on your tongue or inner cheeks. They can also appear on the roof of your mouth, gums, tonsils, or the back of your throat. These areas may look like cottage cheese. They can be painful and may bleed slightly when you scrape them or brush your teeth.
In very bad cases, they can spread into your esophagus and cause:
• Pain when you swallow or difficulty swallowing
• A feeling that food is stuck in your throat or in the middle of your chest
• Fever, if the infection spreads beyond the esophagus
The fungus that causes thrush can spread to other parts of the body, like the lungs, liver, and skin. This happens more often in people with cancer, HIV, or other conditions that weaken the immune system.
How Will I Know if I Have It?
Your dentist or doctor can probably tell by taking a look inside your mouth. Your doctor might also send a tiny sample of the spot to a lab just to make sure.
If the fungus that causes thrush spreads into your esophagus, you may have to have other tests,
like:
• A throat culture (a swab of the back of your throat)
• An endoscopy of your esophagus, stomach, and small intestine
• X-rays of your esophagus
What’s the Treatment?
Thrush is easy to treat in healthy children and adults. But the symptoms may be worse and
harder to treat in people with weak immune systems.
Your doctor will probably prescribe antifungal medications that you’ll have to take for 10 to 14
days. These come in tablets, lozenges, or liquids, and are generally easy to take.
Since the infection can be a symptom of other medical problems, your doctor may also want to
run other tests to rule these out.
How Can I Prevent Thrush?
- Practice good oral hygiene. Brush your teeth at least twice a day and floss at least once a day.
- Get regular dental checkups. Especially if you have diabetes or wear dentures.
- Even if you’re healthy and don’t have dental issues, you should get your teeth cleaned by your dentist every 6
months.
5 ways to prevent grinding your teeth
Symptoms and Effects of Teeth Grinding
- A dull, constant headache originating in the temples
- Teeth that are suddenly more sensitive to heat, cold, or sweetness.
- Soreness on your tongue or the inside of your cheeks, as people who grind their teeth often bite themselves.
- Tired or tight jaw muscles.
What Causes Teeth Grinding?
Doctors don’t have a full understanding of all the causes for grinding your teeth. Stress, anxiety, or even pure force of habit are some common causes. Teeth grinding is very common in childhood, and it can also be caused by sleeping disorders, such as sleep apnea. If your dentist believes your teeth grinding is caused by a sleeping disorder, or another psychological condition, he or she may refer you to a sleep specialist to determine the underlying causes that must be addressed before the teeth grinding can be alleviated. People with overbites or an abnormal alignment of their upper and lower teeth may also experience bruxism.
- Wear a Mouth guard
Mouth guards are the easiest and most typical measures taken against teeth grinding. Your dentist will fit you with a custom plastic mouth guard that you wear every night to sleep. While you’ll probably still move your mouth during the night, the guard acts as a buffer by preventing your teeth from grinding against each other. The soft plastic keeps your teeth safe and prevents further weakening of the enamel.
- Dental correction
In cases where your teeth grinding is caused by a dental problem, the proper procedure to correct the issue might be the right course of action. If you grind your teeth because of a dental misalignment, braces or Invisalign might gradually help you stop by improving the issue. If you have damages to your teeth that cause irregularities in the chewing surfaces, crowns could alleviate your teeth grinding.
- Stress management
For many people, teeth grinding is an instinctual response to stress or anxiety. Often times, if somebody is stressed at work, the subconscious anticipation of the next day’s probable stress can cause them to grind their teeth during their sleep the night before. While your dentist cannot recommend the method of stress management best suited for you, if your teeth grinding is determined to be a result of stress, seek out healthy forms of relieving stress that might help you sleep easier and grind your teeth less.
- Avoid stimulating substances
Certain substances such as caffeinated beverages, or even alcohol, when consumed before bed can increase the frequency of teeth grinding.
- Consult with a sleep specialist
If it is determined that you grind your teeth as a symptom of a sleeping disorder, you may need to consult with a sleep specialist to determine the proper treatment for the disorder. By addressing your sleeping issue at its source, the symptoms of the disorder, including your teeth grinding, should gradually be minimized.
Do you think you grind your teeth at night? If you experience any of the symptoms mentioned above, and have not been able to determine another probable cause, it’s possible that you do. Ask your dentist to examine you for signs that you grind your teeth before your symptoms get worth, and explore which preventative measures are right for you.
Scaling and root planning
Scaling and root planing, also known as conventional periodontal therapy, non-surgical periodontal therapy, or deep cleaning. Dental scaling involves the careful removal of plaque bacteria from the tooth’s surface just below the gumline. The dentist may choose an ultrasonic instrument to scale your teeth. This features a vibrating metal tip combined with a cool water spray. The tip chips tartar away as the water flushes out the pocket.
Dental scaling is typically followed by a procedure known as root planing. Root planing reaches deeper to address the surface of the tooth’s root. This is done in the same manner as scaling. Root planing smooths the surface of the root so the gums can reattach properly.
Dental scaling is routinely performed to help patients with gum disease and excessive plaque buildup. While a standard cleaning will address the surface of the tooth, scaling goes much deeper. If your dentist suggests dental scaling and root planing for your teeth, it’s helpful to know what this means so you can prepare for what’s ahead.
Understanding Scaling
Scaling is a common dental procedure for patients with gum disease. This is a type of dental cleaning that reaches below the gumline to remove plaque buildup. The process of scaling and root planing the teeth is often referred to as a deep cleaning. This treatment goes beyond the general cleaning that you receive with your regular checkup and annual visit.
When Is Dental Scaling Necessary?
Everyone experiences some form of plaque buildup. The saliva, bacteria, and proteins in your mouth form a thin layer that covers your teeth at almost all times. When you eat, tiny particles, acids, and sugars from the food stick to this film, creating a buildup on the teeth known as plaque. The bacteria that lives in this plaque can cause gum disease and tooth decay. Brushing, flossing, and regular dental cleanings will help remove the plaque and prevent more serious problems.
If you have healthy gums, the tissue will fit tightly around the tooth and keep plaque out. However, if gum disease begins to form, this tissue will loosen. Healthy gums attach to the tooth just 1 to 3 millimeters below the gumline. With gum disease, you’ll begin to develop deeper pockets. These can fill with plaque, worsening your problems and causing symptoms like bad breath.
If you have pockets of 4 millimeters or more, your dentist will probably recommend dental scaling to remove the plaque beneath the gumline and help treat the gum disease.
Tooth Sensitivity treatment
Tooth sensitivity is a common dental problem that involves discomfort or pain in teeth when encountering certain substances and temperatures. At least 40 million adults suffer from sensitive teeth in the United States, according to the Academy of General Dentistry.
The pain is often sharp, sudden and it may shoot into the tooth’s nerve endings. Fortunately, sensitive teeth can be treated and the condition can improve.
Causes of tooth sensitivity
“The most common symptom … is a sudden, sharp flash of pain when teeth are exposed to air, cold, sweet, acidic or hot foods,”. Some people may experience tooth sensitivity from brushing or flossing their teeth.
Tooth sensitivity after filling
Some people may experience tooth sensitivity after having a cavity filled or a filling replaced. The tooth decay that causes cavities irritates the tooth, and the filling procedure, while necessary, can lead to further sensitivity. Fortunately, tooth sensitivity after a filling should improve on its own within a few weeks. It may last longer, as much as a few months, but as long as the tooth sensitivity shows gradual improvement, there should be nothing to worry about. Persistent tooth sensitivity, however, may indicate that a root canal is needed.
Sensitive teeth treatment
“Sensitive teeth never completely disappear,”. “Symptoms may be less or even seem to go away for a while but unless the reasons why a person’s teeth become sensitive are completely eliminated the sensitivity will come and go.”
- Desensitizing toothpaste. There are several brands of toothpaste for sensitive teeth available. Your dentist may recommend one or you may have to try different brands until you find the product that works for you. Be sure to use fluoridated toothpaste for sensitive teeth, not tartar-control toothpaste. Try spreading a thin layer of the desensitizing toothpaste on the exposed tooth roots before bed.
- Use a soft-bristled toothbrush.
- Avoid highly acidic foods.
- Use a fluoridated mouthwash daily.
- Avoid teeth grinding. Consider getting a mouth guard.
DENTAL CAMP
THE DENTAL ARCADE organized a free dental check up and awareness camp at S D college sector 32 chandigarh . Over 50 employees and their families were examined and provided with required dentifrices free of cost.
Apart from check-up, the staff were made aware about dental health and hygiene by the team of experts doctors.
Dr Vijita explained that most of the dental diseases can be prevented by simple practice of brushing twice daily with soft brush and regular dental check-up.
She also told that the modern eating habits are one of the biggest reasons for dental problems.
If we regularly visit our dentist and follow good eating habits we can avoid oral problems.
The camp was initiated with dental awareness talk, educating people about common dental ailments, especially stressing on tooth decay and gum diseases and measures to prevent from them.