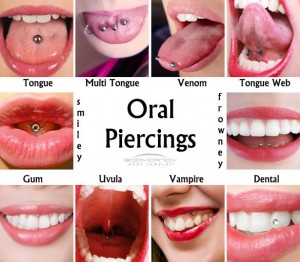
Body piercing is a popular form of self-expression. Oral piercings or tongue splitting may look cool, but they can be dangerous to your health. Oral piercing could also lead to more serious infections, like hepatitis or endocarditis.
If you pierce your tongue, lips, cheeks or uvula (the tiny tissue that hangs at the back of the throat,) it can interfere with speech, chewing or swallowing. It may also cause:
- Infection, pain and swelling. Your mouth is a moist environment, home to huge amounts of breeding bacteria, and an ideal place for infection. An infection can quickly become life threatening if not treated promptly. It’s also possible for a piercing to cause your tongue to swell, potentially blocking your airway.
- Damage to gums, teeth and fillings. biting or playing with the piercing can injure your gums and lead to cracked, scratched or sensitive teeth. Piercings can also damage fillings.
- Hypersensitivity to metals. Allergic reactions at the pierced site are also possible.
- Nerve damage. After a piercing, you may experience a numb tongue that is caused by nerve damage that is usually temporary, but can sometimes be permanent. The injured nerve may affect your sense of taste, or how you move your mouth. Damage to your tongue’s blood vessels can cause serious blood loss.
- Excessive drooling.
If you already have piercings:
- Contact your dentist or physician immediately if you have any signs of infection—swelling, pain, fever, chills, shaking or a red-streaked appearance around the site of the piercing.
- Keep the piercing site clean and free of any matter by using a mouth rinse after every meal.
- Try to avoid clicking the jewellery against teeth and avoid stress on the piercing.
- Check the tightness of your jewellery periodically (with clean hands).
- When taking part in sports, remove the jewellery and protect your mouth with a mouth guard.
- See your dentist regularly, and remember to brush twice a day and floss daily.
Of course the best option is to consider removing mouth jewellery before it causes a problem. Don’t pierce on a whim. The piercing will be an added responsibility to your life, requiring constant attention and upkeep. Talk to your dentist for more information.